After Hospital Care for the Elderly: Tips for Safe and Smooth Recovery
A study published in the Journal of the American Medical Association found that approximately 11.6% of older adults are readmitted to the hospital within 30 days after major surgery.
After hospital care for the elderly involves a comprehensive approach that includes medication management, wound care, physical therapy, and daily living assistance.
All of which highlight the importance of elderly care in promoting recovery and preventing readmissions.
Cooperation prevents complications, reduces readmissions, and supports mobility, nutrition, and emotional well-being.
Recovering from a hospital stay can be challenging for seniors, who often face reduced strength, multiple medications, chronic conditions, and the emotional stress of regaining independence.
In this guide, we’ll explore everything you need to know about after hospital care for the elderly.
From choosing the right care setting and managing recovery at home, to supporting mental and emotional health, and preventing avoidable readmissions.
Thus, let’s get started!
Understanding the After Hospital Care for the Elderly
Recognizing the signs your elderly parent needs help early, such as sudden weakness, confusion, or withdrawal, can make post-hospital recovery safer and more effective.
1. Physical Challenges
Post-hospitalization, many seniors experience significant muscle weakness and reduced mobility due to prolonged bed rest, illness, or surgery.
This decline in physical strength can impede their ability to perform daily activities and increase the risk of falls.
Falls are a leading cause of injury among older adults. Factors such as muscle weakness, joint instability, and environmental hazards contribute to this risk.
2. Medical Challenges
Chronic illnesses like diabetes and vascular diseases can complicate recovery.
Additionally, elderly individuals are more susceptible to chronic wounds, which can be challenging to treat.
3. Emotional and Social Challenges
Hospitalization can lead to feelings of anxiety and depression in older adults.
Addressing these mental health issues through counseling and support is vital for recovery. The prospect of becoming dependent on others can be distressing.
Encouraging autonomy and involving seniors in decision-making can help alleviate these fears.
4. Cognitive Challenges
Delirium is a common postoperative complication in older adults, characterized by sudden confusion and changes in mental status.
It can lead to long-term cognitive decline if not promptly addressed.
Aging is associated with an increased risk of cognitive impairments, including memory loss and difficulty concentrating.
Early detection and intervention are key to managing these challenges.
Step-by-Step Guide to Planning After Hospital Care for the Elderly
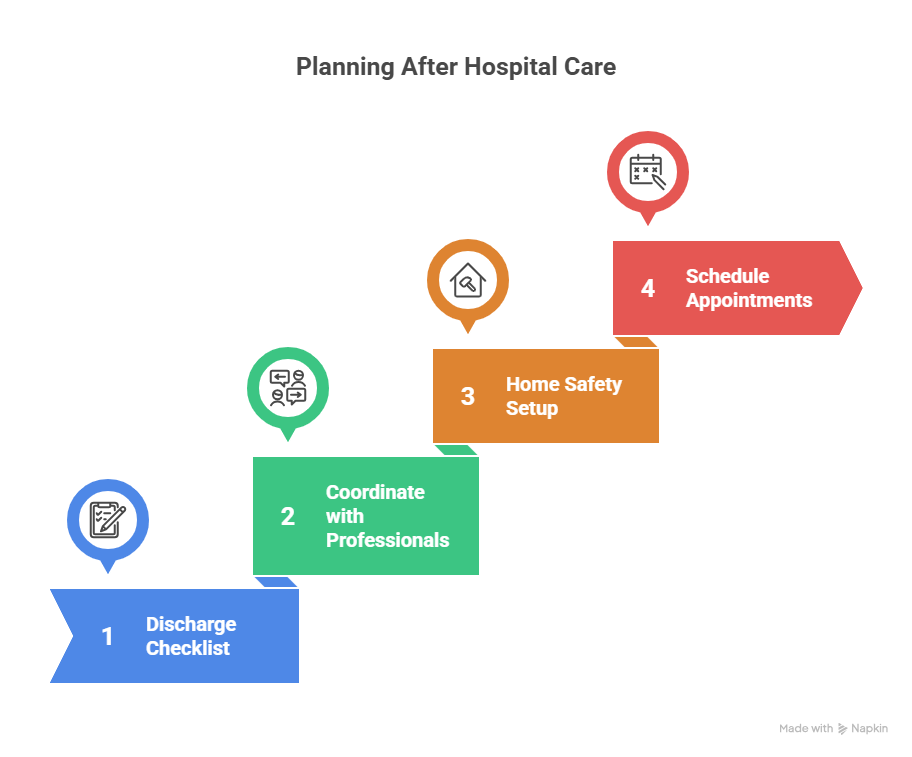
Below is a structured approach to facilitate this process:
Step 1: Discharge Planning Checklist
A clear discharge checklist ensures safe transition and continuity of care.
Review prescribed medications with dosages and side effects, understand the post-discharge care plan, and arrange necessary medical equipment in advance.
Confirm insurance coverage for services and schedule follow-up appointments before leaving the hospital.
Step 2: Coordinate with Hospital Social Workers and Caregivers
Effective discharge planning requires early coordination with social workers, assessment of caregiver support, and thorough education on care needs and emergency procedures.
Providing emotional support throughout the transition helps ensure a safe and confident return home.
Step 3: Set Up Home Safety and Medical Equipment
Install prescribed medical equipment, modify spaces to prevent falls with grab bars and proper lighting, and keep supplies well organized.
Establish a consistent routine for medications, therapy, and rest to maintain stability and comfort.
Step 4: Scheduling Follow-Up Appointments
Schedule appointments before discharge, confirm details and transportation, prepare questions for healthcare providers, and monitor progress.
Care Settings and Options for Post-Hospital Elderly Care
Below is an overview of the primary care options:
1. In-Home Care
In-home care involves trained professionals visiting the individual’s home to provide medical and non-medical assistance.
Services Offered
Assistance with personal care (bathing, dressing, grooming), medication management, meal preparation, light housekeeping, companionship, and prescribed nursing or physical therapy support.
Advantages
- Comfort of staying in a familiar environment
- Personalized care tailored to individual needs
- Promotes independence and dignity
- Flexible scheduling to accommodate family routines
Ideal Candidates: Seniors with moderate medical needs who prefer to remain at home and have family support.
2. Skilled Nursing Facilities (SNFs)
SNFs provide 24/7 medical care and supervision for individuals requiring intensive nursing care or rehabilitation.
Services Offered
Comprehensive care including skilled nursing (wound care, IV therapy), physical, occupational, and speech therapy, medication management, nutritional support, and social or recreational activities.
Advantages
- Continuous medical supervision
- Immediate response to medical emergencies
- Access to specialized therapies and treatments
- Structured environment promoting recovery
Ideal Candidates: Seniors with complex medical conditions, post-surgical recovery needs, or those requiring intensive rehabilitation.
3. Assisted Living Facilities
Assisted living facilities offer a combination of housing, personal care services, and healthcare support in a community setting.
Services Offered
Support with daily activities (bathing, dressing, grooming), medication management, housekeeping and laundry, social and recreational programs, and transportation to medical appointments.
Advantages
- Encourages social interaction and community engagement
- Provides a balance between independence and support
- Access to on-site healthcare services
- Safe and secure environment with 24-hour staffing
Ideal Candidates: Seniors who need assistance with daily activities but do not require intensive medical care.
4. Rehabilitation Facilities
Rehabilitation facilities specialize in helping individuals recover and regain independence after illness, injury, or surgery.
Services Offered
Comprehensive care includes physical therapy for mobility and strength, occupational therapy for daily activities, speech therapy for communication and swallowing, pain management and post-operative support, and psychological counseling.
Advantages
- Intensive therapy programs tailored to individual needs
- Focus on restoring functional independence
- Multidisciplinary team approach to care
- Short-term stay with measurable recovery goals
Ideal Candidates: Seniors recovering from surgery, stroke, or acute illness requiring specialized rehabilitation services.
Choosing between in-home care, assisted living, or skilled nursing often depends on medical needs and family support.
Understanding how to find a care home for elderly loved ones ensures they receive the right balance of comfort, safety, and medical attention.
Key Components of After-Hospital Care for Elderly

Below are the essential components to consider.
1. Medication Management
Key strategies for medication management include reviewing new prescriptions with healthcare providers.
Create a clear administration schedule, and regularly monitor for side effects to report promptly.
2. Physical Rehabilitation
Early physical rehabilitation helps seniors regain strength, maintain independence, and reduce long-term disability.
Incorporate gentle exercises to promote circulation, and use physical, occupational, and speech therapies.
Additionally, include strength-building activities to maintain mobility and prevent falls.
3. Nutrition Support
Adequate nutrition supports healing and prevents malnutrition, which can delay recovery.
Provide easy-to-prepare, nutrient-rich meals, encourage regular meals and hydration, and adjust diets for medical conditions like diabetes or heart disease.
4. Emotional & Social Support
Address anxiety or depression with reassurance and support.
Encourage regular social interactions to reduce loneliness and maintain open communication to meet their emotional needs.
5. Home Safety and Environment
A safe home environment minimizes falls and accidents, which are common among seniors post-discharge.
Conduct a safety assessment to identify hazards like loose rugs or poor lighting.
Install grab bars, maintain clear pathways, and arrange furniture for easy access and mobility.
6. Routine and Stability
Set regular times for meals, medication, rest, and activities to ensure balanced nutrition.
Adequate sleep and overall well-being, while reducing confusion, promote a sense of security.
7. Follow-Up Care
Regular follow-up appointments are vital for monitoring recovery and preventing complications.
Schedule visits with healthcare providers, track health progress, and prepare a list of symptoms or concerns.
Professional Support and Resources for After-Hospital Elderly Care
When exploring reliable support options, families can connect with trusted providers like Gracious Hearts Inc., which offers personalized in-home and post-hospital care.
Below is an overview of key professional resources available.
1. Hospital Discharge Planner
Discharge planners, generally social workers or case managers, ensure a safe transition from hospital to home by assessing medical and psychosocial needs.
They arrange home health support, medical equipment, transportation, follow-ups, and provide patient education.
Effective discharge planning reduces readmissions and improves outcomes.
2. Home Health Agencies
Home health agencies provide medical and supportive care at home under physician supervision, including skilled nursing, therapy services, personal care, and social support.
To choose a provider, consult hospital discharge planners, verify accreditation and licensing, check reviews, and confirm insurance compatibility.
3. Area Agencies on Aging (AAAs) & Community Support
Area Agencies on Aging are state-designated nonprofits that support older adults and their caregivers at local and regional levels.
They offer services such as caregiver support, respite care, meal programs, transportation, and legal or financial guidance.
4. Private Caregiver Platforms
Options include Caring.com and Care.com, which allow searching, interviewing, and hiring for senior care and companionship.
When selecting a caregiver, review qualifications, experience, and references.
Assess compatibility with care needs; discuss availability and rates; and consider trial periods to ensure a good fit.
FAQs
What is the best type of care after hospital discharge?
The best care depends on the senior’s medical needs, mobility, and support system. In-home care is ideal for seniors with moderate medical needs who can safely stay at home with family support. Skilled nursing facilities provide 24/7 medical supervision for complex conditions, while assisted living offers daily living support with social engagement.
How long does post-hospital recovery usually take for seniors?
Recovery times vary based on the type of illness or surgery, age, and overall health. Minor procedures may require a few weeks, whereas major surgeries or strokes can take several months.
What should families watch out for after discharge?
Families should monitor for medication side effects, changes in mobility, signs of infection, depression, anxiety, or confusion. Ensuring home safety, maintaining a routine, and scheduling follow-up appointments are critical to preventing hospital readmission.
Does Medicare cover post-hospital care at home?
Yes, Medicare Part A and Part B cover home health services for eligible patients who are homebound and require intermittent skilled nursing or therapy. Coverage can include nursing care, physical or occupational therapy, and medical social services.
What if I feel unprepared to leave the hospital?
If you feel unready for discharge, communicate your concerns to your healthcare team. You have the right to request additional support or time to prepare. The team can assist in arranging necessary services or addressing any issues to ensure your safety and well-being upon leaving the hospital.
In Summary
Post-hospital care is crucial for seniors to recover safely, regain independence, and prevent complications.
Families and caregivers should focus on medication management, physical rehabilitation, nutrition, emotional support, and home safety.
Imposing professional resources, such as discharge planners, home health agencies, and community support, ensures personalized care and reduces hospital readmissions.
With careful planning, consistent routines, and the right support, seniors can transition smoothly from hospital to home.
