How Long Can You Leave an Elderly Person Alone? Clear Signs & Solutions
According to the CDC, older adults experience over 36 million falls every year. It makes falling the leading cause of injury among seniors.
This alarming statistic is a major reason families urgently ask, “How long can you leave an elderly person alone?”
The answer varies: you can leave an elderly person alone for 2 – 8 hours based on their cognitive health, mobility, and medical needs.
However, adults with dementia should never be left alone due to safety risks.
Before determining safe alone time, it’s essential to evaluate medication schedules, wandering risk, and emergency response ability.
This guide gives clear, practical advice on how long you can leave an elderly person alone.
It explains the key factors to check first, such as physical health, fall risk, mobility, memory, judgment, daily task ability, emotional state, and home safety.
It also covers a range of scenarios, from independent seniors to those with dementia, along with important legal considerations.
Henceforth, let’s get started!
How Long Can You Leave an Elderly Person Alone?
In elderly care, this question matters because every senior has a different risk level based on their health and environment.
A caregiver must assess whether the person can manage each task safely without support.
If a senior has cognitive decline or limited mobility, leaving them unsupervised may increase dangers such as falls, neglect, or even unintentional abuse through lack of needed care.
Ensuring a safe home setup, medical stability, and reliable emergency access helps determine whether a senior can remain alone without compromising their well-being.
| Senior Type | Safe Alone Time | Key Considerations | Risk Level |
| Healthy seniors | 6 – 24 hours | Can manage daily tasks independently | 🟢 Low |
| Mild memory issues | 1 – 4 hours | Periodic check-ins | 🟡 Moderate |
| Dementia | Never | High risk of wandering, accidents | 🔴 High |
| Mobility limitations | Less than 2 hours | Ensure a hazard-free environment | 🔴 High |
Key Factors That Decide How Long Can You Leave an Elderly Person Alone

Each of these influences how safe unsupervised time will be.
1. Cognitive Health (Memory, Alzheimer’s disease, Dementia)
When a senior shows signs of memory loss, wandering behaviour, or impaired decision‑making, their risk of harm increases drastically.
Cognitive impairment reduces the ability to handle unexpected events, medication errors, or disorientation.
If a caregiver sees frequent confusion, forgotten appointments, or unsafe behaviours, longer unsupervised time becomes unsafe.
2. Physical Mobility & Fall Risk
Mobility issues and a history of falls or injuries significantly reduce the safe period a senior can be left alone.
For example, assessments of gait, balance, and mobility aid use (walker, cane) can identify high fall risk.
When an older adult uses a mobility aid or has had a hip fracture, their ability to navigate hazards is limited.
3. Medication Schedules & Medical Conditions
Complex medication regimens, chronic illnesses (heart disease, diabetes, osteoporosis), and frequent changes in treatment increase the need for supervision.
Certain medications raise fall risk or cognitive side effects, requiring review.
If the senior must self‑administer multiple drugs, monitor vital signs, or manage conditions, unsupervised time must be minimal.
4. Emotional Needs & Anxiety
Isolation, anxiety, or depression can worsen cognitive impairment or reduce motivation to perform daily self‑care.
The risk of neglect increases when emotional needs are unmet.
Caregivers should assess whether the person has regular social interactions and support.
5. Home Safety Conditions
Features like grab bars, non‑slip flooring, adequate lighting, and an emergency alert device are essential.
If the home has stairs, clutter, or no monitoring system, the senior’s independence is compromised.
6. Daily Task Management
Evaluate whether the senior reliably handles Activities of Daily Living (ADLs) such as cooking, bathing, dressing, and medication management.
If they struggle with ADLs or cannot adhere to medication schedules, unsupervised time should be very limited.
According to the BC Provincial Health Services Authority’s Fall Prevention Guidelines, difficulty with Activities of Daily Living (ADLs) is a key predictor of a senior’s need for increased supervision.
7. Emergency Preparedness
A working call‑button system, clear caregiver backup, and proximity of emergency response are vital.
Studies show home‑hazard assessment and emergency preparedness reduce fall‑related harm by up to 25 %.
General Guidelines: How Long Can You Leave an Elderly Person Alone Based on Condition
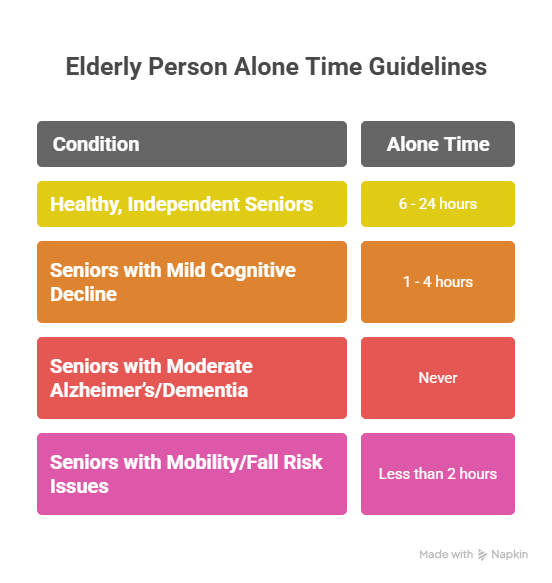
The following guidelines provide a practical framework for caregivers and health professionals to assess risk and plan supervision.
1. Healthy, Independent Seniors
Healthy seniors who can manage their activities of daily living (ADLs), take medications correctly, and move safely around their home may be left alone for 6 – 24 hours.
Regular check-ins or access to emergency contacts are recommended.
2. Seniors with Mild Cognitive Decline
Older adults with some memory lapses or mild judgment issues may be left alone for 1 – 4 hours.
Caregivers should provide reminders, alerts, or periodic check-ins.
Cognitive changes increase risks of medication errors, disorientation, or minor accidents, so supervision should be carefully planned.
3. Seniors with Moderate Alzheimer’s or Dementia
Seniors with moderate or advanced dementia should never be left alone.
Cognitive impairment significantly increases the risk of wandering, accidents, and inability to respond in emergencies.
Continuous supervision or placement in a memory-care environment is essential.
4. Seniors with Mobility or Fall Risk Issues
Those with limited mobility, recent injuries, or a history of falls should be left alone for less than 2 hours, if at all.
Safety Precautions Before Leaving an Elderly Person Alone
These precautions reduce risk, provide peace of mind, and support independence.
1. Keep emergency numbers visible
Post large‑print phone numbers (family, doctor, ambulance) near every landline and program key numbers in their mobile device.
2. Fall prevention
Install grab bars and proper lighting, remove rugs.
According to the Centers for Disease Control and Prevention (CDC), adding grab bars next to the tub and toilet, improving lighting, and removing loose rugs significantly reduce fall risk in older adults.
3. Use smart cameras or monitoring systems
A motion‑activated camera or monitored alert device ensures someone can check in remotely.
4. Schedule regular phone check‑ins
Even healthy seniors benefit from periodic voice check‑ins or video calls. This helps catch early signs of dizziness, confusion, or delayed response.
5. Equip a medical alert device
A wearable pendant or call‑button system gives the senior a direct line to help if they should fall or experience a health emergency.
Signs It’s No Longer Safe to Leave an Elderly Person Alone
Key warning signs include,
1. Forgetting meals or medications: Regularly missing meals or doses may indicate cognitive decline or difficulty managing daily routines.
2. Wandering or confusion: Disorientation, especially in familiar areas, often signals dementia or Alzheimer’s progression.
3. Leaving appliances on: Forgetting to turn off stoves or irons poses serious safety risks.
4. Emotional changes: Increased anxiety, withdrawal, or depression can affect judgment and self-care.
5. Frequent falls: Recurrent slips or instability suggest declining mobility, balance, or coordination.
Alternatives to Leaving an Elderly Person Alone

When leaving a senior alone is unsafe, several supportive options can ensure safety and companionship.
1. Part-time caregivers: Respite care gives family caregivers a needed break while ensuring seniors receive attentive support.
Organizations like Gracious Hearts, Inc. provide trained, compassionate caregivers who assist with daily tasks, offer companionship, and maintain a safe home environment.
2. Adult daycare programs: These centers provide structured activities, social engagement, and medical supervision.
They help seniors stay active and connected while giving caregivers relief during the day.
3. Companionship services: Companion caregivers provide emotional support, conversation, and assistance with daily routines.
4. Remote-monitoring technology: Smart cameras, motion sensors, and telehomecare systems enable caregivers to monitor well-being remotely, providing alerts for falls or other emergencies.
Legal and Ethical Considerations When Leaving Elderly People Alone
Knowledge of relevant laws ensures seniors’ safety and protects caregivers from potential liability.
State Laws & Adult Neglect Regulations
- Many U.S. states define elder neglect as failing to provide supervision, food, hygiene, or protection from harm.
- Neglect or abandonment may carry criminal penalties, particularly if it results in serious injury or death.
- Certain professionals, including healthcare workers, are legally required to report suspected elder abuse to Adult Protective Services (APS).
- Federal programs such as the Elder Justice Act (42 U.S. Code § 3058i) support prevention, coordination, and intervention in elder abuse and neglect.
Duty of Care for Family Caregivers
- Family members who assume responsibility for an elderly person have a legal duty of care to act reasonably and prevent harm.
- Failing to provide supervision or meet basic needs can lead to civil or criminal liability if the elder is injured.
- Ethically, caregivers must balance respect for the senior’s independence with their safety and vulnerability.
- Some states have filial responsibility laws that require adult children to support parents in need.
Frequently Asked Questions (FAQs)
1. How long can an elderly person be left alone overnight?
The safe duration depends on their health, cognitive function, and mobility. Healthy seniors with no fall risk may stay alone longer, but those with dementia, memory issues, or mobility challenges should not be left unsupervised overnight.
2. Can I leave my elderly parent alone during the day?
Daytime alone time is possible for seniors who can manage activities of daily living (ADLs), medication, and basic home safety. Short check-ins or monitoring systems are recommended.
3. What safety devices help seniors when left alone?
Helpful devices include medical alert systems, motion sensors, grab bars, stove alarms, and smart home monitoring systems.
4. When should I hire in-home care?
Consider in-home care if the senior struggles with ADLs, experiences frequent falls, shows cognitive decline, or has health conditions requiring supervision. Even short-term or part-time care can provide safety, companionship, and peace of mind.
5. Is it illegal to leave a bedridden person alone?
Leaving a bedridden person alone can be legally risky. While laws vary by state or country, leaving someone who cannot care for themselves without supervision may be considered elder abuse or neglect, and could result in civil or criminal liability. Always assess the person’s level of dependency and provide appropriate support or professional care.
Conclusion
Leaving an elderly person alone safely depends on their health, mobility, cognitive function, and home environment.
Therefore, caregivers must assess each situation carefully and provide the appropriate level of supervision.
Proactive planning, safety precautions, and emotional support are essential to protect seniors and maintain their independence.
Ultimately, understanding how long can you leave an elderly person alone requires thoughtful evaluation and individualized care planning.
