Wound Care for Elderly Thin Skin: 6-Step Guide
Did you know that in long-term care settings, as many as 41.5% of elderly residents experience skin tears due to fragile skin?
Wound care for elderly thin skin goes beyond treating injuries. It helps prevent infection, lowers hospital visits, and supports faster healing for vulnerable seniors.
As skin thins with age, seniors are more prone to tears, bruises, pressure injuries, and chronic wounds, making gentle yet effective care essential.
That means cleaning wounds carefully with mild soap and water, applying non-adherent dressings, and keeping the wound moist with hydrogel or petroleum-based ointments.
Protecting fragile skin with soft bandages, avoiding adhesive tapes, and changing dressings every 24 – 48 hours not only reduces infection risk but also promotes healing.
In this comprehensive guide, you’ll find complete guidance on wound care techniques, protective dressing options, hydration and nutrition strategies, and proven prevention methods to keep elderly skin healthier.
Therefore, let’s dive into it!
Understanding Elderly Thin Skin
Elderly thin skin, also known as dermatoporosis, is a condition characterized by fragile, translucent skin that tears easily.
According to a study published in Frontiers in Endocrinology, dermatoporosis is prevalent among the elderly, with women being more affected than men.
This vulnerability increases the risk of bruising, skin tears, and delayed wound healing.
Causes of Skin Thinning in Older Adults
1. Natural Aging: As we age, the skin loses collagen and elastin. It leads to a thinner epidermis and dermis. This reduction in skin thickness makes the skin more susceptible to injury.
2. Medications: Long-term use of corticosteroids and blood thinners can weaken the skin and blood vessels. Eventually, it increases the risk of skin tears.
3. Chronic Illnesses: Conditions like diabetes and vascular diseases can impair circulation and immune response. That leads to slower wound healing and increased skin fragility.
The combination of reduced collagen production, decreased skin thickness, and impaired circulation contributes to the fragility of elderly skin.
These factors make the skin more prone to tears and slower to heal after injury.
Types of Wounds Common in Elderly Thin Skin
As skin thins with age, elderly individuals become more susceptible to various types of wounds. Those are,
1. Skin Tears
Skin tears are the most frequent wounds in the elderly, especially those with thin or fragile skin.
These are traumatic wounds caused by friction, shear, or blunt force, which lead to the separation of the skin layers.
They often occur on the upper extremities and can be classified into three types:
- Type 1: No skin loss, with the flap still attached.
- Type 2: Partial flap loss, with some tissue loss.
- Type 3: Total flap loss, leaving an open wound.
According to Wounds International, skin tears are prevalent in long-term care settings, with incidences ranging from 1.1% to 41.2% based on the care setting
2. Bruises and Abrasions
Elderly individuals often experience bruising due to fragile blood vessels and thinner skin.
Even minor trauma can cause blood vessels to rupture. Aging skin also becomes more prone to abrasions, which are superficial wounds caused by friction.
These injuries can be painful and may lead to complications if not properly managed.
3. Chronic Wounds
Chronic wounds, such as diabetic foot ulcers and venous leg ulcers, are common among the elderly.
These wounds often result from underlying health conditions like diabetes, poor circulation, or venous insufficiency.
They are characterized by slow healing and can lead to serious complications if not effectively managed.
4. Pressure Ulcers (Bedsores)
Pressure ulcers, also known as bedsores, occur when prolonged pressure on the skin reduces blood flow to the area. It leads to tissue damage.
They commonly develop over bony prominences such as the heels, sacrum, and elbows. Elderly individuals, especially those with limited mobility, are at high risk.
5. Minor Cuts and Scrapes
While minor, these injuries can be more severe in elderly individuals due to thinner skin and slower healing processes.
Even small cuts or scrapes can lead to infections if not properly cleaned and dressed.
6. Bruises That Break the Skin
In some cases, bruises can progress to skin tears or ulcers, especially if the skin is already fragile.
These injuries require prompt attention to prevent further complications.
Step-by-Step Wound Care for Elderly Thin Skin
The following step-by-step guide outlines best practices for managing wounds in elderly individuals with thin skin.
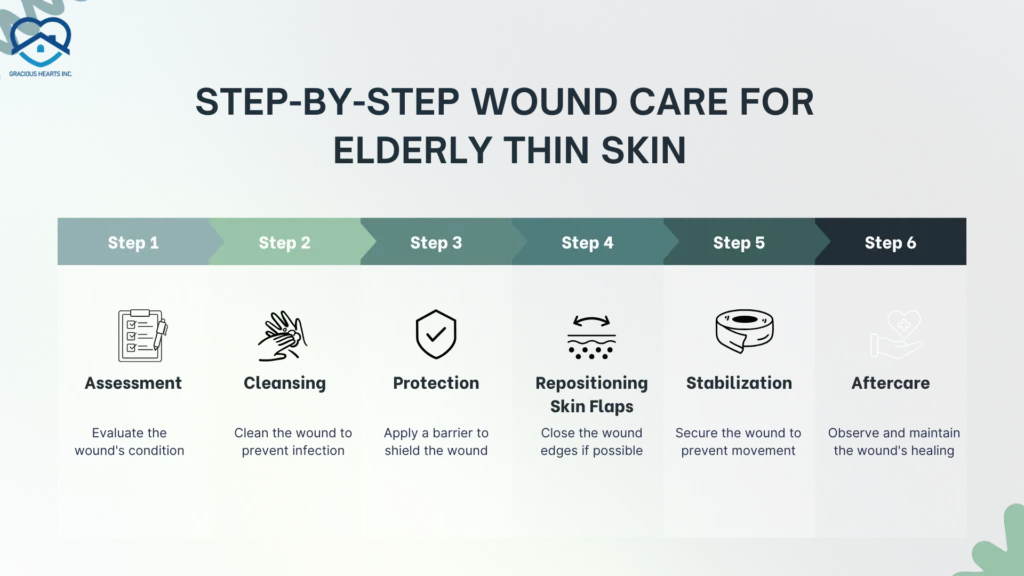
Step 1: Assessment
At first, carefully inspect the wound for size, depth, and any signs of infection such as redness, swelling, or discharge.
Next, assess the surrounding skin for signs of maceration, dryness, or irritation. Then, record the wound’s characteristics, including location, dimensions, and any changes over time.
Step 2: Cleansing
Use mild soap and lukewarm water or sterile saline to cleanse the wound. Avoid harsh antiseptics like hydrogen peroxide or alcohol, as they can further irritate fragile skin.
Use a soft, sterile gauze pad to gently cleanse the wound, removing any debris or exudate.
Carefully pat the wound and surrounding skin dry with a clean, soft towel.
Step 3: Protection
Apply non-adherent dressings, hydrocolloid, or foam dressings to protect the wound and maintain a moist healing environment.
Always avoid adhesive tapes and use soft bandages or tubular netting. This can prevent further trauma to fragile skin.
Gently secure the dressing in place and ensure it is not too tight to avoid compromising circulation.
Step 4: Repositioning Skin Flaps
If the wound involves a skin flap, gently reposition it to cover the wound bed.
For minor skin tears, consider using steri-strips or skin glue to approximate the edges. For more severe wounds, sutures may be necessary.
Regularly assess the viability of the skin flap, looking for signs of necrosis or infection.
Step 5: Stabilization
Ensure the dressing remains in place and intact, and change it as needed or when it becomes soiled.
Minimize movement or activities that could dislodge or disrupt the dressing. Watch for signs of infection, such as increased redness, swelling, or purulent discharge.
Step 6: Monitoring & Aftercare
Conduct daily assessments of the wound and surrounding skin for any changes or signs of complications.
Change the dressing according to the wound’s condition and the dressing’s manufacturer’s recommendations.
If the wound shows signs of infection, does not improve, or worsens over time, seek medical attention promptly.
Choosing the Right Dressings for Elderly Thin Skin
The choice between adhesive and non-adhesive dressings, as well as the selection of specific types like hydrogel and foam dressings, can significantly impact healing outcomes.
1. Non-Adhesive vs. Adhesive Dressings
Non-adhesive dressings are designed to protect wounds without sticking to the wound bed. It minimizes the trauma during dressing changes.
These are particularly beneficial for fragile skin, as they reduce the risk of further injury.
In contrast, adhesive dressings can securely hold the dressing in place but may cause discomfort or skin damage upon removal, especially on sensitive skin.
2. Hydrogel Dressings
Hydrogel dressings are moisture-rich and provide a soothing effect on dry or necrotic wounds.
They facilitate autolytic debridement, promote the removal of dead tissue, and maintain a moist environment conducive to healing.
However, they may not be suitable for heavily exudating wounds due to their low absorbency.
3. Foam Dressings
Foam dressings are highly absorbent and provide cushioning. These are ideal for moderate to heavily exuding wounds.
They help maintain a moist wound environment, which is essential for optimal healing.
Some foam dressings incorporate antimicrobial agents to reduce infection risk and feature soft silicone adhesives that minimize pain and skin trauma during dressing changes
Preventing Infection in Elderly Wounds
Proper hygiene, vigilant monitoring, and preventive strategies are essential to keep skin healthy and reduce complications.

1. Hand Hygiene
Proper handwashing before and after wound care is critical to reduce infection risk.
Use clean gloves when handling dressings or touching the wound.
2. Monitoring for Signs of Infection
Watch for redness, swelling, warmth, increased pain, pus, or foul odor.
Fever or sudden malaise may indicate a systemic infection requiring immediate medical attention.
3. Clean Dressing Practices
Change dressings as recommended (usually every 24 – 48 hours or when soiled).
Avoid reusing dressings and always use sterile or clean materials.
Prevention of Wounds and Skin Tears in Elderly Individuals
Follow the given preventive measures in daily routines to prevent the risk of skin tears and related complications.
1. Daily Skin Hydration Routines
Maintaining skin hydration is crucial for elderly individuals, as aging skin tends to lose moisture and elasticity. It increases the risk of tears.
Implementing a daily moisturizing routine can help preserve skin integrity. Focus on areas prone to dryness or friction, such as forearms, hands, and lower legs.
Apply a fragrance-free, emollient-rich moisturizer to the skin twice daily, especially after bathing, to lock in moisture and prevent dryness.
Use lukewarm water and a mild, pH-balanced cleanser to avoid stripping natural oils. Avoid scrubbing; gently pat skin dry with a soft towel.
Apply broad-spectrum sunscreen (SPF 30 or higher) to exposed areas, even on cloudy days.
2. Clothing and Protective Gear
Protective clothing serves as a physical barrier against potential injuries and environmental factors that can lead to skin tears.
Utilize padded arm and leg sleeves to cushion vulnerable areas, particularly for individuals with a history of skin tears.
Dress in long-sleeved shirts, long pants, and knee-high socks to shield the skin from abrasions.
Ensure the use of non-slip, well-fitting shoes to prevent falls and related injuries.
3. Nutrition for Healthy Elderly Skin
Adequate nutrients and hydration can enhance wound healing, improve elasticity, and reduce the risk of skin tears.
- Protein: Protein is essential for cell regeneration and tissue repair. Include lean meats, fish, eggs, dairy, legumes, and nuts in daily meals to support skin strength and recovery from injuries. (NIH)
- Vitamin C: Supports collagen synthesis. It improves skin structure. Found in citrus fruits, berries, and peppers.
- Vitamin E: Acts as an antioxidant, protects skin from damage. Sources include nuts, seeds, and spinach.
- Vitamin A: Promotes cell turnover and repair. Found in carrots, sweet potatoes, and leafy greens.
- Hydration: Encourage adequate water intake to maintain skin moisture and elasticity.
4. Foods That Support Healing
Zinc-rich foods (pumpkin seeds, beans) aid tissue repair.
Omega-3 fatty acids (salmon, flaxseeds) reduce inflammation and improve skin barrier function.
5. Environmental Modifications
Creating a safe living environment is essential to minimize the risk of accidents that can lead to skin injuries.
Eliminate clutter, secure loose rugs, and pad sharp furniture edges to prevent accidental bumps and falls.
Install adequate lighting in hallways, staircases, and bathrooms to improve visibility and reduce trip hazards.
Provide grab bars in bathrooms and handrails along stairways to offer support and stability.
6. Fall Prevention Strategies
Falls are a leading cause of skin tears in the elderly. Implementing fall prevention strategies can significantly reduce this risk.
Conduct regular fall risk assessments and adjust care plans accordingly.
Ensure the use of mobility aids, such as walkers or canes, as needed, and provide training on their proper use.
Encourage participation in balance and strength training exercises to enhance mobility and coordination.
When to Seek Medical Attention for Elderly Skin Issues
Seek professional care if you observe any of the following.
1. Signs of Infection
If a wound becomes increasingly painful, swollen, produces pus, or is accompanied by a fever, it may indicate an infection.
Infections can spread quickly in older adults and require immediate medical intervention.
2. Deep, Large, or Non-Healing Wounds
Wounds that are deep, large, or fail to heal after several days may require professional treatment.
Such wounds can lead to complications like delayed healing or chronic ulcers.
3. Heavy Bleeding That Doesn’t Stop
If a wound continues to bleed despite applying pressure for 10 – 15 minutes, it’s essential to seek emergency medical care. Persistent bleeding can lead to significant blood loss and other serious health issues.
4. Recurrent Skin Tears
Frequent skin tears may indicate underlying health problems such as nutritional deficiencies, vascular issues, or the need for medication adjustments.
It’s advisable to consult a healthcare provider to address these recurring incidents.
For elderly individuals requiring specialized care for fragile skin, Gracious Hearts Inc. in Arizona provides specialized support for seniors, ensuring safety, personalized attention, and optimal healing.
FAQs
Why do elderly people have thin skin that tears easily?
As people age, the skin loses collagen, fat, and elasticity, making it thinner and more fragile. This natural aging process reduces the skin’s ability to heal and increases the risk of tears and bruising.
How do you treat a skin tear in the elderly?
First, gently clean the wound with mild saline or water, then reposition any skin flap if possible. Cover it with a non-stick, sterile dressing to protect against infection. Avoid adhesive bandages that can damage fragile skin.
What is the best dressing for fragile elderly skin wounds?
Non-adherent dressings such as silicone-coated foam, hydrogel, or soft gauze are best. They cushion the wound, keep it moist for healing, and prevent further skin damage during dressing changes.
Should elderly skin tears be left open or covered?
Wounds on elderly thin skin should always be covered with a breathable, non-stick dressing. Leaving them uncovered increases the risk of infection and delays healing.
What vitamins help elderly skin heal faster?
Vitamins C, D, E, and zinc are important for wound healing. A balanced diet rich in protein and hydration also supports faster recovery in older adults with fragile skin.
Bottom Line
Elderly individuals with thin, fragile skin require gentle, consistent care to promote healing and prevent complications.
Implementing a comprehensive approach that includes daily skin hydration, proper nutrition, and vigilant wound management can significantly enhance skin health and recovery outcomes.
Gentle, consistent care, such as using emollient-rich moisturizers, mild cleansers, and protective clothing, helps maintain skin integrity and prevents tears.
Timely medical consultation for signs of infection, non-healing wounds, or recurrent skin tears ensures prompt intervention and optimal healing.
With gentle care, prevention, and the right support, fragile skin can heal strong, and every senior can enjoy comfort!
